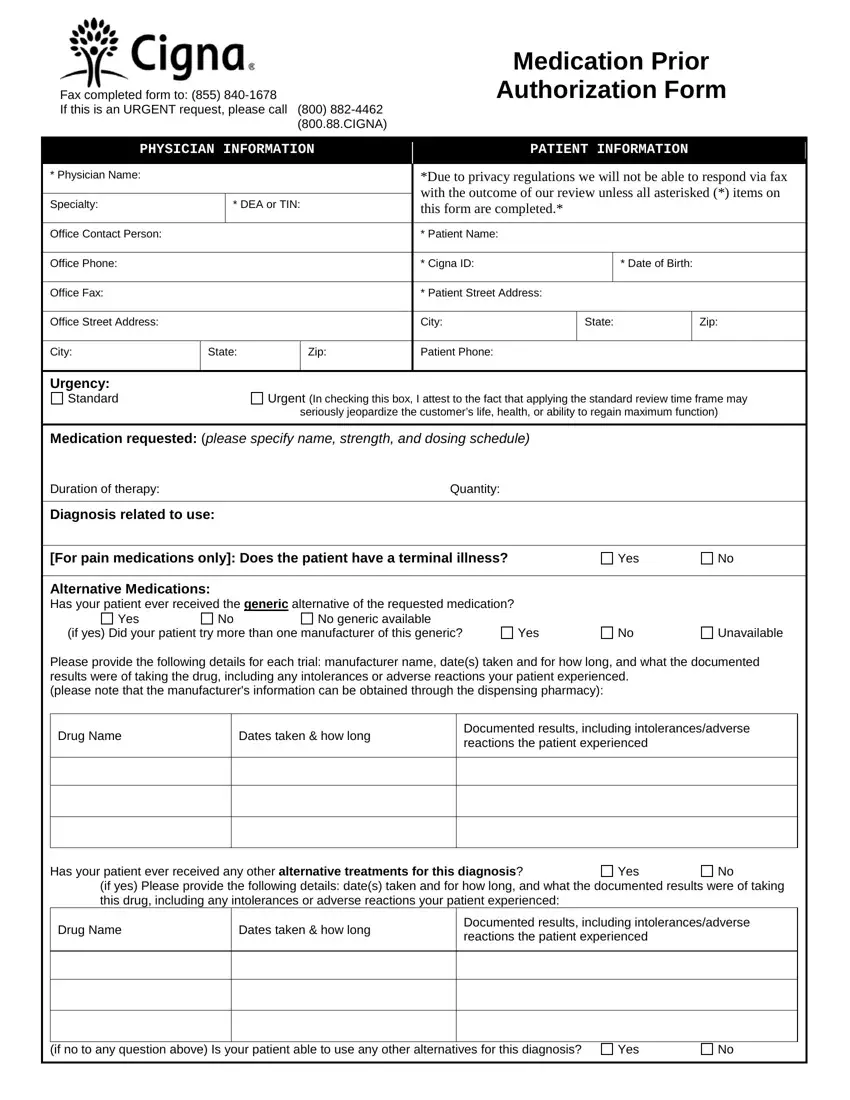
Need to submit a prior authorization for Viagra through Cigna? Download the necessary form directly from Cigna’s website – a link is provided below. This significantly reduces processing time.
Ensure your form is complete. Specifically, include all patient demographics, prescribing physician information, and a detailed diagnosis justifying the medication. Missing information delays approvals. Carefully review the instructions on the form itself for specific requirements.
Fax the completed form to the appropriate Cigna number, as listed on the form. Confirm receipt via phone call or email after faxing to avoid any potential misunderstandings. Following this process ensures prompt handling of your request.
Expect a response within the timeframe Cigna specifies. If you haven’t received a response within that period, contact Cigna directly using their member services line. Keep your reference number handy for quicker resolution.
For the most up-to-date information and direct access to the Cigna prior authorization form, visit [Insert Cigna’s website link here]. This link provides the most current version of the form and contact details.
- Cigna Viagra Prior Authorization: A Comprehensive Guide
- Gathering Necessary Information
- Submitting Your Request
- Appealing a Denial
- Alternative Options
- Understanding Cigna’s Prior Authorization Process for Viagra
- Gathering Required Information
- Finding and Completing the Cigna Viagra Prior Authorization Form
- Successfully Navigating Cigna’s Viagra Prior Authorization System
- Completing the Cigna Prior Authorization Form
- Submitting Your Prior Authorization Request
- Troubleshooting Common Issues
- Contacting Cigna
- Alternative Treatments
- Keeping Records
Cigna Viagra Prior Authorization: A Comprehensive Guide
First, confirm your Cigna plan covers prescription drugs. Check your Summary of Benefits and Coverage (SBC) or contact Cigna directly. Next, obtain a prescription from your doctor. This prescription must clearly state the medical necessity for Viagra. Your physician should explain how Viagra addresses your specific condition and why alternative treatments are unsuitable.
Gathering Necessary Information
Before submitting your prior authorization request, gather all required documentation. This typically includes the prescription, your doctor’s detailed justification for Viagra, and your insurance information. Cigna may request additional medical records or tests depending on the case. Provide clear and concise information, making it easy for the reviewer to understand.
Submitting Your Request
Submit your prior authorization request through Cigna’s online portal or by fax, using the contact information provided on your insurance card. Follow all instructions carefully; incomplete or poorly documented submissions frequently result in delays. Retain a copy of your submission and tracking number for future reference. Expect a decision within a reasonable timeframe specified by your plan.
Appealing a Denial
If your prior authorization is denied, review the denial letter carefully. Understand the reasoning behind the rejection. You may appeal this decision by providing additional supporting documentation demonstrating the medical necessity of Viagra for your condition. Follow the instructions outlined in the denial letter regarding the appeals process. Don’t hesitate to contact Cigna directly to discuss your appeal.
Alternative Options
Consider exploring alternative treatments with your doctor. They may suggest other medications or therapies to address your condition. Open communication with your healthcare provider is key to finding the best solution for your health needs.
Understanding Cigna’s Prior Authorization Process for Viagra
First, confirm Viagra is covered under your specific Cigna plan. Coverage varies by plan type and individual policy details. Check your Summary of Benefits and Coverage document or contact Cigna member services.
Gathering Required Information
Next, collect necessary information for the prior authorization request. This usually includes your prescription, doctor’s contact information, and possibly medical records detailing the medical necessity for Viagra. Prepare this documentation beforehand to expedite the process.
Submit your prior authorization request through Cigna’s online portal or by fax, following the instructions provided on your Cigna website. Ensure all required fields are accurately completed. Use clear, concise language on all supporting documentation.
Cigna typically processes requests within a few business days; however, processing times can vary. Track your request’s status through Cigna’s online portal or by contacting member services. If you haven’t heard back within the expected timeframe, follow up with Cigna directly. Be prepared to provide your request’s tracking number.
If your request is denied, understand Cigna’s rationale. Discuss options with your doctor, such as appealing the decision or exploring alternative treatments covered by your plan.
Finding and Completing the Cigna Viagra Prior Authorization Form
First, contact your doctor. They’ll initiate the prior authorization process with Cigna. They will likely provide you with the necessary form or direct you to Cigna’s online portal.
Next, access Cigna’s provider portal. You or your doctor should be able to find the appropriate form within their online system. Look for documents related to prior authorization or pre-certification for medications.
Carefully review the form. Fill out all required fields completely and accurately. Ensure your name, date of birth, policy number, and prescription details are correct. Provide your physician’s information as well. Any missing data can delay the approval.
Gather supporting medical documentation. This may include your medical history, relevant test results, and your doctor’s rationale for prescribing Viagra. Attach these to the completed form.
Submit the completed form through the designated method. The Cigna portal usually provides instructions for submission. If submitting via mail, use certified mail for tracking.
Track the status of your request. Use the online portal or contact Cigna directly to check on the status of your prior authorization. Follow up if you don’t receive a response within a reasonable timeframe.
Note: Cigna’s processes may change. Always refer to their official website for the most up-to-date information.
Remember: This is guidance. Specific requirements may vary. Consult your doctor or Cigna directly for any ambiguities.
Successfully Navigating Cigna’s Viagra Prior Authorization System
Gather all necessary patient information before starting the process. This includes the prescription, diagnosis codes, and complete patient demographics. Accuracy is key!
Completing the Cigna Prior Authorization Form
Use the most current form available on the Cigna website. Double-check all entries for accuracy. Incomplete forms delay processing.
- Clearly indicate the medication (Viagra), dosage, and duration of treatment.
- Provide detailed clinical justification for Viagra’s use, referencing specific guidelines if applicable.
- Ensure your physician’s signature and contact information are legible and correct.
Submitting Your Prior Authorization Request
Cigna accepts submissions electronically through their provider portal. This is generally the fastest method.
- Log in to your provider portal.
- Locate the prior authorization section.
- Upload the completed and signed form along with all supporting documentation.
- Track your submission’s status online.
Troubleshooting Common Issues
If your request is denied, promptly review the denial letter for specific reasons. Address these issues and resubmit with corrected information. Common reasons for denial include missing information or insufficient clinical justification.
Contacting Cigna
If you encounter problems or require clarification, contact Cigna’s provider services directly. Use their dedicated phone number or online portal for faster assistance. Have your patient’s information ready.
Alternative Treatments
In the event of an unsuccessful prior authorization, discuss alternative treatment options with the patient and their physician. This proactive approach benefits both parties.
Keeping Records
Maintain detailed records of all communication and submissions. This helps resolve future issues and ensures compliance.