Always follow your doctor’s instructions precisely. Prednisone dosage varies greatly depending on the specific condition being treated, your individual health, and your response to the medication. Typical starting doses range from 5mg to 60mg daily, often administered in divided doses. Your physician will carefully adjust your dosage based on your progress.
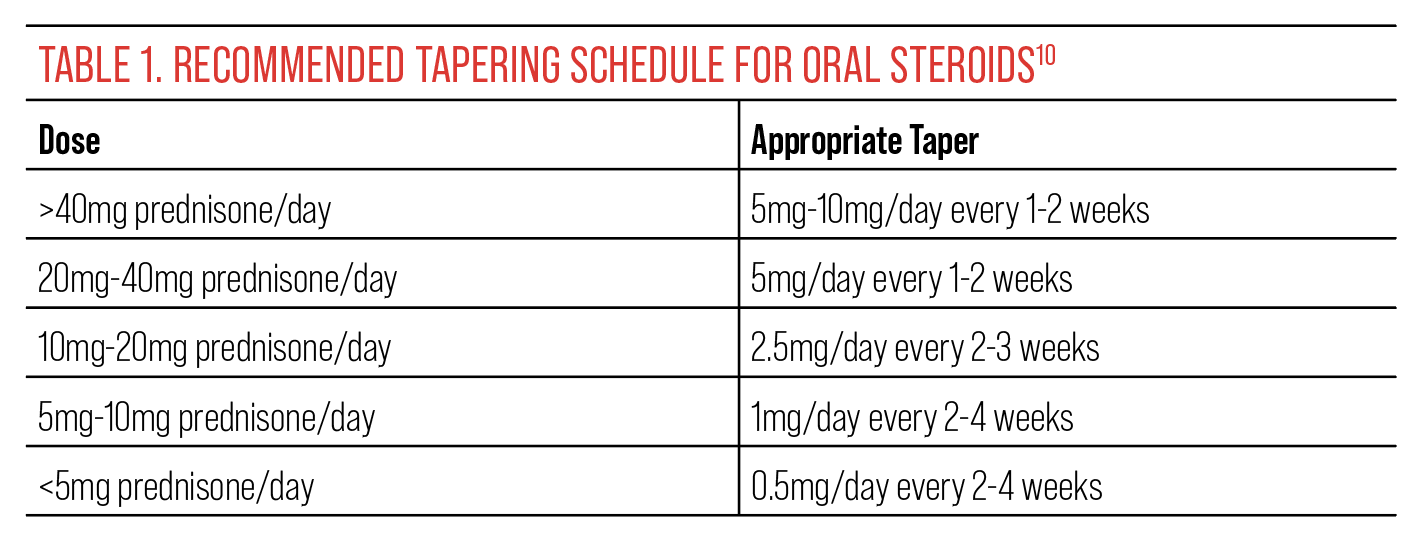
Never abruptly stop taking Prednisone. Sudden cessation can lead to serious withdrawal symptoms. Your doctor will create a tapering schedule to gradually reduce your dose, minimizing the risk of adverse effects. This usually involves slowly decreasing the daily amount over several weeks or months.
Common side effects include increased appetite, weight gain, mood changes, and increased blood sugar. Report any unusual or concerning symptoms to your healthcare provider immediately. Regular monitoring of blood pressure, blood sugar, and potassium levels is often necessary, especially during long-term treatment. Understanding potential side effects is critical for managing your treatment effectively.
Prednisone interacts with numerous medications. Be sure to inform your doctor of all medications, supplements, and herbal remedies you are currently taking. This is particularly important to avoid potential drug interactions and ensure safe and effective treatment. This proactive communication is your best safeguard.
- Prednisone Usage and Dosage: A Comprehensive Guide
- Tapering Off Prednisone
- Common Side Effects and Management
- Long-Term Use and Monitoring
- What is Prednisone and How Does it Work?
- How Prednisone Works
- Common Conditions Treated with Prednisone
- Prednisone Dosage: Starting, Maintenance, and Tapering
- Administering Prednisone: Oral and Other Methods
- Alternative Administration Routes
- Potential Side Effects of Prednisone
- More Serious Side Effects
- Managing Prednisone Side Effects
- Prednisone and Interactions with Other Medications
- Common Drug Interactions
- Other Potential Interactions
- What to Do
- Disclaimer:
- Long-Term Prednisone Use and Risks
- Bone Health
- Metabolic Changes
- Immune System Suppression
- Other Potential Risks
- When to Consult a Doctor Regarding Prednisone
Prednisone Usage and Dosage: A Comprehensive Guide
Always follow your doctor’s instructions precisely. Prednisone dosage varies greatly depending on the condition being treated and your individual health. Typical starting doses range from 5mg to 60mg daily, often administered in a single dose or split throughout the day. Your physician will determine the best schedule for you.
Tapering Off Prednisone
Never stop taking prednisone abruptly. Sudden cessation can cause serious withdrawal symptoms. Your doctor will create a tapering schedule, gradually reducing your dose over several weeks or months. This ensures a smoother transition and minimizes adverse effects. Typical tapering involves decreasing the dosage by small increments at regular intervals, as directed by your physician.
Common Side Effects and Management
Potential side effects include increased appetite and weight gain, mood changes, insomnia, fluid retention, and increased blood sugar. Maintaining a healthy diet and regular exercise can help mitigate these. Discuss any concerns with your doctor; they can suggest strategies for managing side effects or adjusting your treatment plan.
Long-Term Use and Monitoring
Long-term prednisone use requires close monitoring by your doctor. Regular blood tests and check-ups are necessary to assess your overall health and monitor for potential complications. Open communication with your healthcare provider is key to ensuring safe and effective treatment. Your doctor will adjust the dosage or treatment plan as needed, based on your individual response and any observed side effects.
What is Prednisone and How Does it Work?
Prednisone is a corticosteroid medication, a synthetic version of the hormone cortisol your body naturally produces. It powerfully reduces inflammation and suppresses your immune system.
How Prednisone Works
Prednisone works by binding to receptors within your cells. This triggers a cascade of events, ultimately decreasing the production of inflammatory substances like prostaglandins and leukotrienes. This reduction in inflammation leads to noticeable improvements in symptoms associated with many inflammatory conditions.
Simultaneously, Prednisone dampens your immune response. This property makes it effective in treating autoimmune diseases where your immune system mistakenly attacks your own body. However, this immunosuppressive effect also increases your susceptibility to infections.
Remember, Prednisone mimics a natural hormone, so its effects are widespread. It can influence metabolism, blood sugar levels, and fluid balance, requiring careful monitoring by your doctor.
Common Conditions Treated with Prednisone
Prednisone treats various inflammatory and autoimmune conditions. Rheumatoid arthritis, a chronic inflammatory disorder affecting joints, often benefits from prednisone’s anti-inflammatory action, reducing pain and swelling. Lupus, a complex autoimmune disease causing widespread inflammation, similarly responds to prednisone’s immunosuppressive effects, managing flare-ups and protecting organs.
Asthma, a respiratory condition marked by airway inflammation, uses prednisone to reduce inflammation and improve breathing. Allergic reactions, ranging from mild skin rashes to life-threatening anaphylaxis, find relief in prednisone’s ability to quickly suppress the immune response. Certain inflammatory bowel diseases like Crohn’s disease and ulcerative colitis utilize prednisone to manage inflammation and improve symptoms.
Some cancers benefit from prednisone as part of a combination therapy to control tumor growth and alleviate symptoms; however, this should only be done under strict medical supervision. Prednisone also aids in treating certain eye conditions such as uveitis, an inflammation of the uvea, a part of the eye. Finally, some severe skin conditions like pemphigus and dermatomyositis respond well to its anti-inflammatory properties.
Disclaimer: This information is for general knowledge and does not constitute medical advice. Always consult a healthcare professional for diagnosis and treatment. Prednisone has potential side effects; discuss them with your doctor before starting treatment.
Prednisone Dosage: Starting, Maintenance, and Tapering
Your doctor determines your Prednisone dosage based on your specific condition and response to treatment. Starting doses often range from 20 to 60 milligrams daily, potentially higher in severe cases. This initial high dose quickly reduces inflammation.
Maintenance doses, if needed, are significantly lower. Your doctor will carefully adjust your dosage to the lowest effective amount, typically reducing the daily dose gradually. This might involve taking prednisone every other day or alternating between high and low doses. The goal is to manage symptoms with the smallest amount of medication to minimize side effects.
Tapering Prednisone is crucial to avoid withdrawal symptoms. Never stop taking Prednisone abruptly. Your doctor will create a gradual tapering schedule, usually reducing your dose by small increments, such as 5 milligrams every few days or weeks. This slow reduction allows your body to adjust naturally. The tapering period can last several weeks or even months, depending on your individual needs and the initial dose.
Closely monitor your condition and report any changes to your doctor. They may adjust the tapering schedule accordingly. Remember, consistent communication with your healthcare provider is paramount for safe and effective Prednisone management.
Administering Prednisone: Oral and Other Methods
Prednisone is typically administered orally, usually as a tablet or capsule. Swallow the medication whole with a full glass of water. Avoid crushing or chewing the tablets, as this can alter the drug’s release and absorption. Follow your doctor’s instructions precisely regarding dosage and frequency; never adjust the dosage without consulting your physician. Some patients find taking prednisone with food minimizes stomach upset.
Alternative Administration Routes
While oral administration is standard, prednisone can also be given intravenously (IV) or intramuscularly (IM) in specific situations, such as severe illness or inability to swallow. IV administration provides rapid absorption, useful in emergencies. IM injection provides slower, sustained release, though less common for prednisone. A healthcare professional will administer these injections. Your doctor will determine the most appropriate route based on your individual needs and health status. Always communicate any concerns or challenges with medication administration to your doctor or pharmacist.
Potential Side Effects of Prednisone
Prednisone, while highly effective, carries potential side effects. These vary depending on dosage and duration of treatment. Common side effects include increased appetite leading to weight gain, mood changes such as irritability or anxiety, and insomnia. You might also experience fluid retention, resulting in swelling in your legs and ankles. Some people develop acne or experience thinning skin.
More Serious Side Effects
Less frequent, but more serious side effects demand immediate medical attention. These include increased risk of infection due to immune system suppression, high blood sugar (hyperglycemia), and increased blood pressure. Gastrointestinal issues such as stomach ulcers or pancreatitis are also possibilities. Long-term use can increase the risk of osteoporosis and cataracts. Always report any concerning symptoms to your doctor.
Remember to discuss any pre-existing conditions with your physician before starting Prednisone. They can help manage potential side effects and ensure your safety. Regular monitoring of blood pressure, blood sugar, and bone density may be necessary, particularly with prolonged treatment.
Managing Prednisone Side Effects
Communicate openly with your doctor about any side effects. They can adjust your dosage or prescribe medication to alleviate symptoms.
To counter weight gain, focus on a balanced diet rich in fruits, vegetables, and lean protein. Regular exercise is also key.
For insomnia, establish a consistent sleep schedule. Avoid caffeine and alcohol before bed. Your doctor might suggest a sleep aid if needed.
Manage increased blood sugar through dietary changes and regular monitoring. Your doctor may recommend medication to control blood glucose levels.
High blood pressure can be addressed with dietary modifications (reducing sodium intake) and, if necessary, with blood pressure medication.
Mood swings are common. Consider stress-reduction techniques like meditation or yoga. Talk to your doctor about potential medication adjustments.
Here’s a summary table to help you track your side effects and potential solutions:
| Side Effect | Management Strategies |
|---|---|
| Weight gain | Balanced diet, regular exercise |
| Insomnia | Consistent sleep schedule, avoid caffeine/alcohol before bed, consult doctor about sleep aids |
| Increased blood sugar | Dietary changes, blood glucose monitoring, potential medication |
| High blood pressure | Dietary modifications (reduce sodium), potential blood pressure medication |
| Mood swings | Stress-reduction techniques, discuss medication adjustments with doctor |
Remember, these are general suggestions. Always consult your doctor for personalized advice and treatment.
Prednisone and Interactions with Other Medications
Always inform your doctor about all medications you take, including over-the-counter drugs, herbal remedies, and supplements, before starting Prednisone. This includes vitamins and aspirin.
Common Drug Interactions
- Warfarin (Coumadin): Prednisone can reduce the effectiveness of warfarin, increasing your risk of blood clots. Your doctor will need to monitor your INR (International Normalized Ratio) closely.
- Digoxin (Lanoxin): Prednisone may increase the levels of digoxin in your blood, leading to toxicity. Your doctor will monitor your digoxin levels.
- Diabetes Medications (Insulin, Metformin): Prednisone can raise your blood sugar levels, requiring adjustments to your diabetes medication. Regular blood sugar monitoring is crucial.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Combining Prednisone with NSAIDs like ibuprofen or naproxen increases the risk of stomach ulcers and bleeding. Your doctor may recommend alternatives.
- Potassium-wasting diuretics: Prednisone can cause potassium loss, and using it with potassium-wasting diuretics can worsen this, leading to dangerously low potassium levels. Your doctor may monitor your potassium levels and adjust your medications.
Other Potential Interactions
Prednisone can interact with many other medications. These include:
- Immunosuppressants
- Antibiotics
- Anticonvulsants
- Oral contraceptives
- Drugs affecting the central nervous system
What to Do
Open communication with your doctor is paramount. Report any new or worsening symptoms while taking Prednisone. Regular blood tests may be necessary to monitor your response to the medication and detect any potential interactions.
Disclaimer:
This information is for general knowledge and does not constitute medical advice. Always consult your healthcare provider for personalized guidance regarding Prednisone and its potential interactions with other medications.
Long-Term Prednisone Use and Risks
Long-term prednisone use, defined as more than three weeks, significantly increases your risk of several adverse effects. These risks vary depending on dosage and duration of treatment. For example, high doses over extended periods pose a substantially greater threat than low doses for a shorter time.
Bone Health
Prolonged prednisone use weakens bones, increasing the risk of osteoporosis and fractures. This happens because prednisone interferes with calcium absorption and bone formation. Doctors often recommend calcium and vitamin D supplements, along with weight-bearing exercise, to mitigate this risk. Regular bone density testing may also be necessary.
Metabolic Changes
Prednisone can disrupt your metabolism, leading to weight gain, increased blood sugar (hyperglycemia), and increased cholesterol levels. These changes raise the risk of developing type 2 diabetes and cardiovascular disease. Careful monitoring of blood sugar and cholesterol levels is crucial, along with dietary modifications and potentially medication adjustments to control these effects. Regular check-ups with your doctor are vital.
Immune System Suppression
Prednisone suppresses your immune system, making you more vulnerable to infections. This increased susceptibility can range from minor infections to serious illnesses. Practicing good hygiene, getting vaccinated, and promptly seeking medical attention for any signs of infection are essential precautions.
Other Potential Risks
Other potential long-term side effects include glaucoma, cataracts, increased blood pressure, fluid retention, mood swings, and skin thinning. Regular eye examinations and blood pressure monitoring are recommended during long-term prednisone use. Open communication with your physician is vital to manage these risks effectively and adjust treatment accordingly.
When to Consult a Doctor Regarding Prednisone
Contact your doctor immediately if you experience any of the following:
- Severe stomach pain
- Difficulty breathing or shortness of breath
- Rapid heartbeat
- Swelling in your face, legs, or ankles
- Muscle weakness
- Increased thirst or urination
- Vision changes
- Severe headache
- Easy bruising or bleeding
- Signs of infection, such as fever, chills, or persistent cough
Schedule a doctor’s appointment if you notice:
- Weight gain
- Mood changes, such as increased anxiety or irritability
- Sleep disturbances
- Increased appetite
- Acne or skin changes
- Increased blood sugar levels (if you have diabetes)
Regular monitoring is crucial. Your doctor should check your blood pressure, blood sugar levels (if applicable), and other relevant indicators during your treatment. Follow your doctor’s instructions carefully for tapering off Prednisone; abruptly stopping can be harmful. Report any new or worsening symptoms promptly.
- Maintain open communication with your doctor throughout your treatment.
- Keep a record of your symptoms and any changes in your health.
- Be aware of potential side effects and don’t hesitate to seek medical attention if you are concerned.